Abstract
Background: Primary central nervous system lymphoma (PCNSL) is an aggressive extranodal subtype of diffuse large B-cell lymphoma (DLBCL). High-dose methotrexate (HD-MTX)-based regimen is the first-line treatment of PCNSL, with or without the anti-CD20 antibody rituximab, remaining to be suboptimal due to unstable response and short effective remission time. Genetic alterations often occur in the chronic active B-cell receptor signaling featured by MYD88 and CD79B which mediate the response to BTK inhibition (BTKi) in PCNSL. Orelabrutinib is a novel, potent, highly selective BTK inhibitor with a high CSF concentration. This study aims to investigate optimal combination dose of Orelabrutinib in combination with Rituximab, Methotrexate, and Dexamethasone (ORMD) as well as safety and efficacy of the regimen.
Methods: This was a phase 1, investigator-initiated, dose-escalation study of ORMD, being conducted at Huashan Hospital, Fudan University (ClinicalTrials.gov identifier: NCT05036577). It was planned to enroll 12-15 patients with newly diagnosed PCNSL to the regimen of orelabrutinib and MTX combined with the fixed dose of rituximab(R) and dexamethasone(D). Eligible patients must have histopathologically confirmed PCNSL-DLBCL by biopsy of brain lesions and be aged 18-75 years with adequate organ functions. Patients were treated for 6-8 cycles of induction therapy with 21 days per cycle, receiving rituximab (375mg/m2 on day 1), dexamethasone (10-15mg on d1-d4), MTX (d2, 3.5g/m2 or 5g/m2), and orelabrutinib (once daily, after MTX clearance, 150mg/d, or 200mg/d), followed by orelabrutinib maintenance up to one year among CR/CRu patients. The primary objective was to determine the maximum tolerated dose (MTD) of the combination of orelabrutinib and MTX with R and D and investigate the safety and tolerability of this regimen using Bayesian Optimal Interval (BOIN) waterfall design to determine rule of dose escalation and movement among dose combination matrix to identify MTD contour. DLT was defined by the occurrence of severe toxicities during the first cycle: any grade 4 hematologic toxicity, grade 3 febrile neutropenia and grade 3 thrombocytopenia with hemorrhage, or any grade 3 non-hematologic toxicity that failed to respond to supportive therapy and possibly related to orelabrutinib and/or MTX (assessed according to NCI CTCAE V5.0). The secondary objectives included ORR/CR(u) and PFS/OS. Baseline tissue/CSF samples and sequential CSF/plasma samples were collected for targeted NGS and pharmacokinetics evaluation as exploratory objectives.
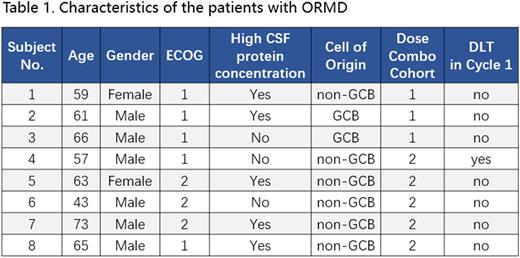
Results: Eight patients were enrolled from October 2021 to June 2022 as the preliminary analysis set. The median age was 62 year (range: 43-73) and six patients were male. All the patients with histologically confirmed DLBCL (6 non-GCB subtypes and 2 GCB subtypes) had completed at least one cycle of ORMD treatment and were evaluable for DLT. The median cycle of ORMD was one (range: 1-7). No DLT occurred among first three patients in cohort 1 (Orelabrutinib: 150mg/MTX: 3.5g/m2) and dose escalation was allowed to cohort 2 (Orelabrutinib: 200mg/MTX: 3.5g/m2). In cohort 2, 5 patients were dosed in total, and Gr 3 lung infection was observed in patient #4 during cycle 1, was deemed as a DLT. Another four patients were enrolled in the same cohort according to BOIN design algorithm and no DLT was identified, allowing to escalate to cohort 3 (Orelabrutinib:200mg/MTX:5g/m2). No Gr 4 AE had been observed. The most common adverse events were lymphopenia (Gr 3 in 4 case) and hyperglycemia (Gr 3 in 1 case). No atrial fibrillation, hypertension, or bleeding was observed by the cut-off date. The study is ongoing. Further results will be updated as data becomes mature.
Conclusions: ORMD regimen preliminarily demonstrated predictable and manageable safety profile in newly diagnosed PCNSL patients with 200mg/d orelabrutinib and 3.5g/m2 MTX to date. MTD contour not reached and further evaluation continues. Longer follow-up is needed regarding efficacy, biomarker, and more safety data
Disclosures
Chen:Takeda Pharmaceutical Company Limited: Research Funding, Speakers Bureau.
OffLabel Disclosure:
Orelabrutinib is a novel selective Bruton Tyrosine kinase(BTK) inhibitor. BTK inhibitors are highly effective in B cell NHL which carried MYD88 and/or CD79b mutations. PCNSL has highfrequency of MYD88/CD79b mutations.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal